#First co-authors
*Equal corresponding authors
Although coronavirus disease 2019 (COVID-19) is primarily a respiratory infection, mounting evidence suggests that the gastrointestinal tract is involved in the disease, with gut barrier dysfunction and gut microbiota alterations related to disease severity. Increased gut barrier permeability can cause a local inflammation and change circulating inflammatory thresholds leading an enhanced leakage of bacterial products to the circulation.
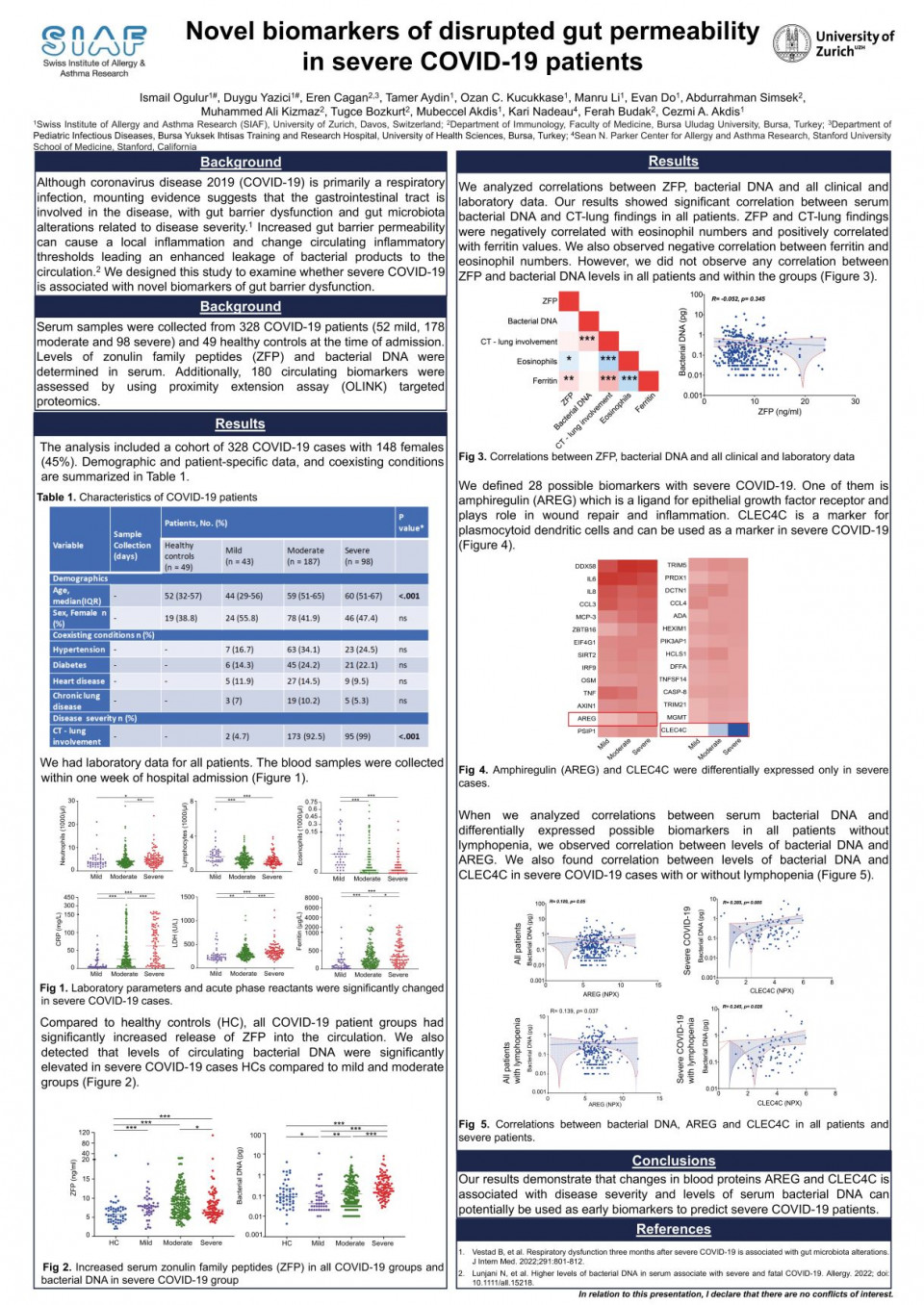
We designed this study to examine whether severe COVID-19 is associated with novel biomarkers of gut barrier dysfunction. Serum samples were collected from 327 COVID-19 patients (52 mild, 178 moderate and 98 severe) and 49 healthy controls at the time of admission. Levels of zonulin family peptides (ZFP) and bacterial DNA were determined in serum. Additionally, 180 circulating biomarkers were assessed by using proximity extension assay (OLINK) targeted proteomics.
Compared with healthy controls, all COVID-19 patient groups including mild (P < 0.001), moderate (P < 0.001) and severe (P < 0.001) had significantly increased levels of circulating ZFP. We also detected that levels of circulating bacterial DNA were significantly elevated in severe COVID-19 patients compared with healthy controls (P < 0.001), with mild COVID-19 patients (P < 0.001) and with moderate COVID-19 patients (P < 0.001). Interestingly, there was no correlation between the levels of circulating bacterial DNA and ZFP in COVID-19 patients. Compared to healthy controls, we defined 39 proteins as potential biomarkers in COVID-19 severity. When we analyzed patients with lymphopenia, it was found that severe COVID-19 is associated with higher levels of bacterial DNA and markers of inflammation and immune response including IL-10, MCP-3 and AREG in the circulation.
Our results demonstrate that changes in blood proteins associated with disease severity and levels of ZFP and bacterial DNA can potentially be used as early biomarkers to predict severe COVID-19 patients.