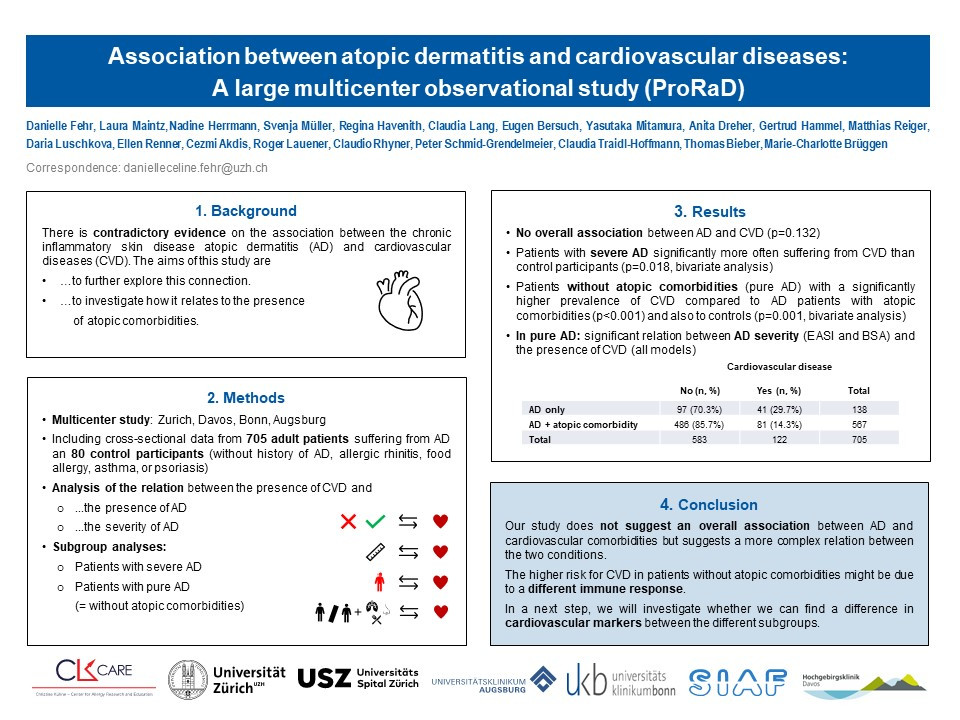
Methods:
This observational multicenter study included cross-sectional data of 705 adult patients suffering from AD and 80 control participants (without history of AD, allergic rhinitis, food allergy, asthma, or psoriasis) of the ProRaD cohort (Zürich, Davos, Bonn, Augsburg). EASI, body surface area (BSA), SCORAD and objective SCORAD were used to grade AD severity. The presence of atopic, cardiovascular, and metabolic conditions was assessed by a dermatologist. Cardiovascular risk factors (age, sex, smoking habits, physical activity, body mass index) as well as other clinical and epidemiological data were asked in a standardized questionnaire. The main outcome variable for statistical analysis was the presence of CVD, the main dependent variables being the presence of AD and the severity of AD respectively. In the minimally adjusted model, we controlled for age and sex, in the fully adjusted model for all the above-mentioned cardiovascular risk factors.
Results:
Our analysis did not show an overall association between AD and cardiovascular outcomes. However, patients with severe AD were significantly more often suffering from CVD than control participants (24.4% [29/119] vs. 10.0% [8/80]). Furthermore, AD patients without atopic comorbidities (pure AD) had a significantly higher prevalence of CVD compared to AD patients with atopic comorbidities (29.7% [41/138] vs. 14.3% [81/567]). Yet, both associations could not be confirmed in the adjusted models. In patients with pure AD, there was a statistically significant relation between the severity of AD (EASI and BSA) and the presence of cardiovascular comorbidities, which could be confirmed in multivariate analyses.
Conclusions:
Our study does not suggest an overall association between AD and cardiovascular comorbidities but suggests a more complex relation between the two conditions: A higher BSA involvement may be indicative of a stronger pro-inflammatory type 1 reaction in pure AD and represent a risk factor for CVD. Conversely, a more prominent type 2 response (clinically evidenced by atopic comorbidities) might counterbalance this tendency.