Background
T cell metabolism and reprogramming post cellular activation influence their proliferation, differentiation, function, and memory formation. This phenomenon has been extensively evaluated in the context of cancer and diabetes but knowledge gaps pertaining to T cell metabolic reprogramming in type 2 inflammation and allergy still exist. Hence, we aimed to study memory CD4+ T effector (Teff) and regulatory (Treg) cell metabolism in allergy to improve our understanding of metabolic mechanisms and their role in facilitating the allergy phenotype.
Methods
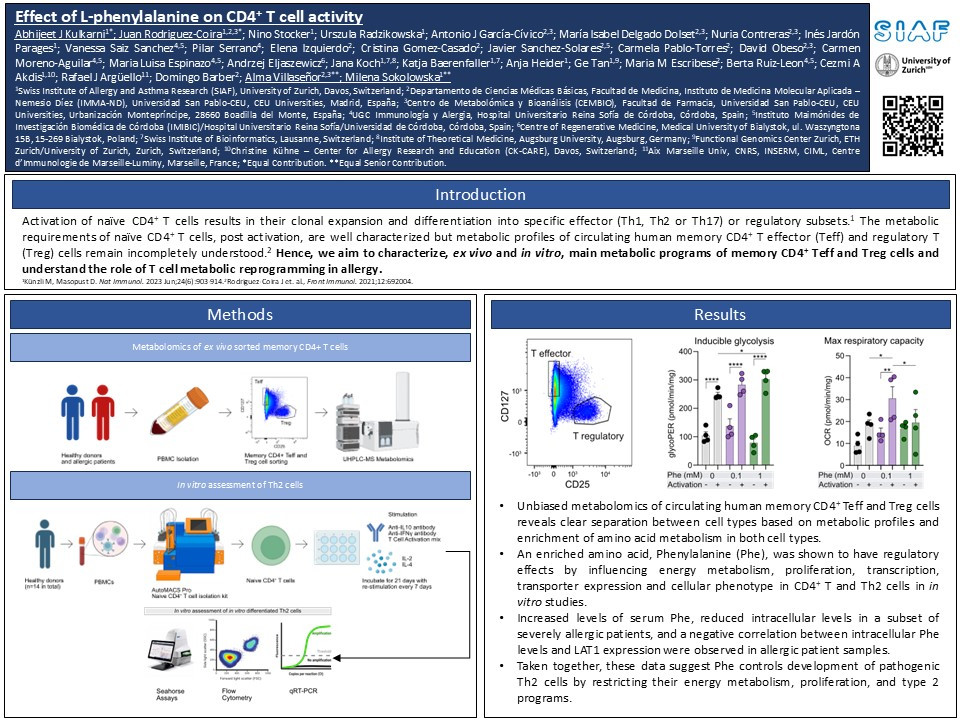
In our analysis, we employed several techniques for the ex vivo and in vitro assessment of multiple CD4+ T cell populations to study their metabolism. Memory CD4+ Teff and Treg cells were sorted from allergic patients and healthy controls using fluorescence-activated cell sorting (FACS) and subjected to untargeted metabolomics by UHPLC-QToF mass spectrometry. Subsequently, to assess and characterize CD4+ T cell or T cell subset energy metabolism, proliferation, phenotype, and functionality under the influence of L-Phenylalanine we used Seahorse extracellular acidification rate assays (Seahorse), qRT-PCR, flow cytometry, Single Cell ENergetIc metabolism by profilIng Translation inhibition (SCENITH), CFSE based proliferation, siRNA based knockdown experiments, and carried out analysis of previously published transcriptomics datasets comparing T cells between allergic patients and healthy controls.
Results
In healthy subjects, memory CD4+ Teff cells could be completely differentiated from memory Treg cells based on their metabolomes although their composition showed high similarity in terms of metabolite classes. Overrepresentation analysis of metabolomics data emphasized amino acid metabolism in both cell types including L-phenylalanine (Phe) metabolism. Considering this observation and very limited number of studies evaluating the effect of Phe on CD4+ T cell metabolism, we decided to focus on this amino acid and study its effect on CD4+ T, Th2 and Treg cells. In in vitro studies, we observed that supplemented Phe enhanced memory CD4+ T cell glycolysis while limiting their oxidative phosphorylation. Furthermore, Phe limited memory CD4+ T cell proliferation by an interleukin-4-induced-1 oxidase (IL4I1)-dependent mechanism which was confirmed by siRNA knockdown studies. Not only were observations replicated in Th2 cells, but we also observed Phe, at high doses, significantly limited the transcription of activation markers, type 2 cytokines, and key metabolic enzymes such as mTOR, CD69, BACH2, BATF, IL-4, IL-5, IL-13, PKM2, PFKFB3, and IDH2 in in vitro differentiated Th2 cells. Additionally, supplementation of Phe limited the expression of CD161, a documented pathogenic Th2a cell marker. Finally, we also observed increased levels of Phe in the sera of severe allergic patients combined with reduced intracellular levels in memory CD4+ Teff cells and reduced expression of key Phe transporter, LAT1, in severe allergic patients.
Conclusion
In summary, these data collectively suggest Phe plays a critical role in preventing the development of pathogenic Th2a cells which could be potentially exploited for the development of therapy in the context of allergy.