Approximately 36 million surgeries for bone fracture repair happen annually. However, up to 10% of fractures suffer from delayed healing or non-union. Bone fracture non-union is classified as a failure of bone healing at least 6 months after fracture fixation. It's a challenging clinical problem, with treatment approaches varying depending on the underlying causes. Treatment of infected non-union demands intra- and postoperative protocols that differ fundamentally from those in case of aseptic non-union. In case of septic non-union caused by biological or mechanical failure, the treatment takes between 3-6 months. However, in case of an infection the treatment takes up to 2 years with quite a burden for the patients. Nevertheless, confirming infection as the underlying cause is challenging, particularly in low grade cases without clear infection signs. Preoperative blood testing would be valuable in diagnosing infectious causes and facilitate early initiation of appropriate treatment. The aim of this study was to characterize blood cells (peripheral blood mononuclear cells (PBMCs)) from patients with septic and aseptic non-union and compare with patients with uneventful healing.
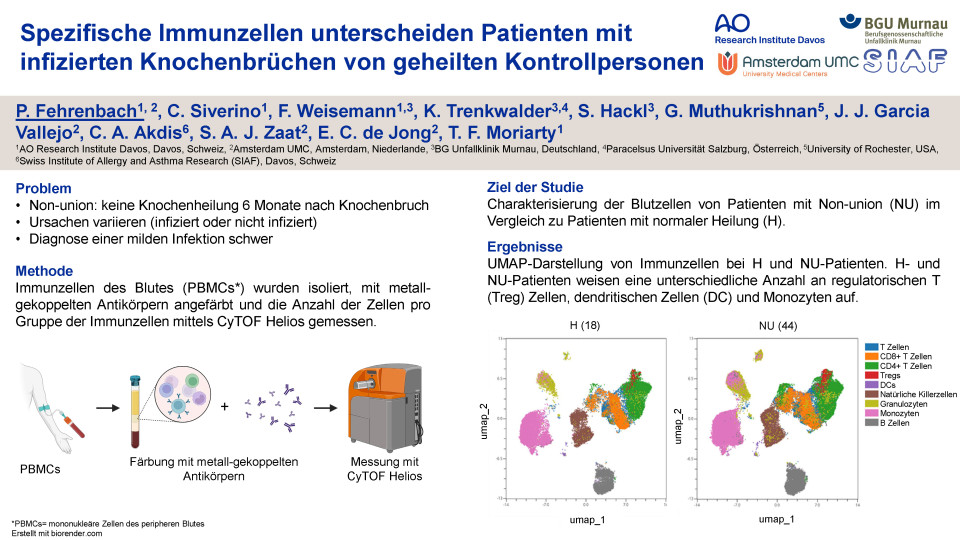
Patients were recruited from eight level-one trauma centres in Germany, after appropriate ethical approval. Blood from healed (n=18), septic non-union (n=20) and aseptic non-union (n=24) patients was taken before surgical revision for routine implant removal or treatment of septic or aseptic non-union respectively. PBMCs were characterized by their expression of specific blood cell surface markers using high-dimensional mass cytometry with a total of 43 markers.
The cell groups investigated originated from both the adaptive and the innate immune system. Innate immune cells were monocytes, granulocytes and NK cells. T and B cells were examined as part of the adaptive immune system. CD4+ T cells assist in the activation of B cells to secrete antibodies and assist in the activation of CD8+ T cells to kill infected cells.
Among the different cell types analyzed, CD4+ T cells subgroups showed most of the significant differences between the three groups. T regulatory cells regulating the response of immune cells. These cells were increased in aseptic (p=0.0119) non-union patients compared to healed patients. Furthermore, Th1 cells were elevated in septic non-union patients compared to both healed (p=0.0004) and aseptic non-union patients (p=0.0074). Th1 cells are playing an important role in inflammatory responses and cell-mediated immunity. Activation marker CD38 was decreased in CD4+ T cells in aseptic non-union patients compared to healed patients (p=0.0004). Exhaustion (PD-1, OX-40 and ICOS) and activation markers (HLA-DR and CD69) showed no significant differences in CD4+ and CD8+ T cells. Additionally, monocytes were significantly increased in septic non-union patients compared to both healed (p=0.0094) and aseptic non-union patients (p≤0.0001). Monocytes are involved in processes that occur during an immune response, both inflammatory and anti-inflammatory.
In summary, septic non-union patients show an elevated number of monocytes and Th1 cells and reflect a state of infection. In addition, T helper cell subsets seem to play a fundamental role in non-union patients, as they all differ between healed and non-union patients. These findings suggest that preoperative blood testing might be used to provide distinct biomarkers to identify non-union patients.
Quiz question
Welcher Zelltyp ist in Non-Union Patienten im Vergleich zu geheilten Patienten erhöht?
NK Zellen
regulatorische T Zellen
B Zellen