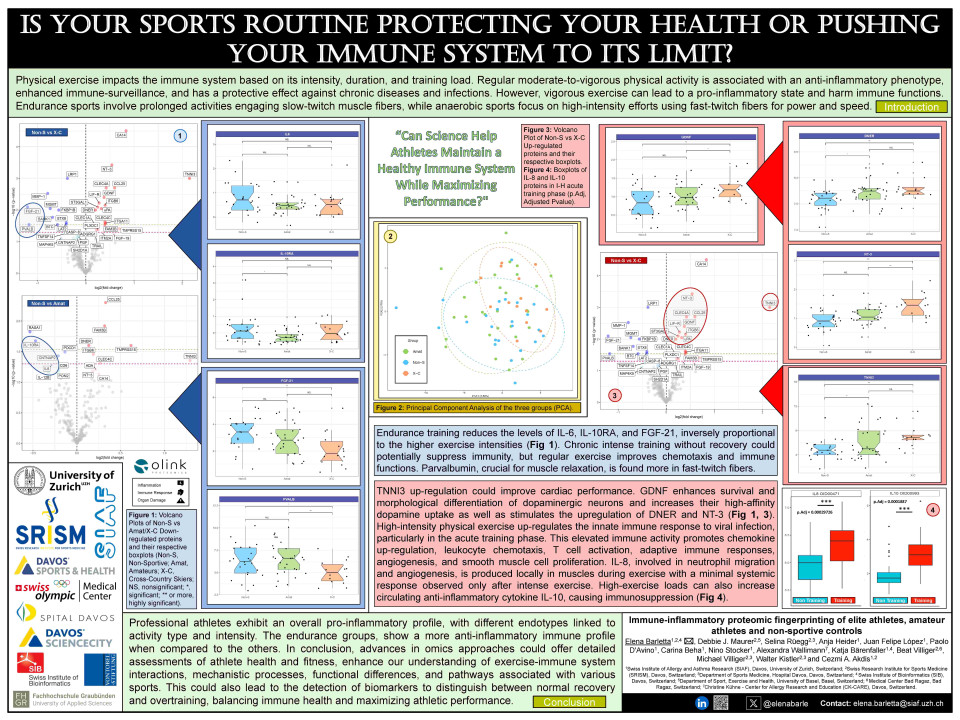
Physical exercise is known to impact our immune system in various ways, depending on its intensity, duration and training load. Many factors have been implicated in the ability of exercise to modulate the immune response, such as variations in circulating levels of cytokines and chemotactic factors, changes in adhesion molecules, the generation of reactive oxygen species as well as nutritional status, which is of main interest for immune-metabolic studies. Regular moderate-to-vigorous physical activity is associated with an anti-inflammatory phenotype, enhanced immunosurveillance, and has a protective effect against chronic non-communicable diseases, infections and likely cancer. The reduction in adipose tissue and changes in hormonal, myokine, and cytokine levels that result from regular exercise are thought to be the main contributors to its anti-inflammatory effects.
On the other hand, vigorous exercise can potentially lead to an overall pro-inflammatory state and have detrimental effects on immune function. This is especially the case for elite athletes, whose long-term training loads often exceed the recommended upper levels for physical activity and who tend to face further stressors that can impair adequate immune responses, particularly during competitions and heavy training phases. Additionally, endurance sports involve prolonged activities engaging slow-twitch muscle fibers, while anaerobic sports focus on high-intensity efforts using fast-twitch fibers for power and speed. In its 2016 consensus statement, the International Olympic Committee pointed out the importance of further investigation into the relationship between training load and risk of illness to minimize illness-related training absence, decrease in performance, and overtraining syndrome in professional athletes. Studies have shown that illnesses during competitions and tournaments are more frequently observed in winter sports athletes.
In this study, we used proximity extension assay (PEA)-based targeted proteomics to investigate the impact of different levels of exercise on organ damage-, immune response-, and inflammation-related proteins in three different cohorts: winter sport athletes, amateur athletes and non-sportive controls. Based on our results, endurance training reduces the levels of IL-6, IL-15, and FGF-21, inversely proportional to the higher exercise intensities. Chronic intense training without recovery could potentially suppress immunity, but regular exercise improves chemotaxis and immune functions. Parvalbumin, crucial for muscle relaxation, is found more in fast-twitch fibers and TNNI3 up-regulation could improve cardiac performance. The PI3K-Akt pathway is able to support cardiac hypertrophy and its changes, together with MAPKs, are activated by IL-18, promoting pro-inflammatory cytokine production, which are important for tissue regeneration. High-intensity physical exercise up-regulates the innate immune response to viral infection, particularly in the acute training phase. This elevated immune activity promotes chemokine up-regulation, leukocyte chemotaxis, T cell activation, adaptive immune responses, angiogenesis, and smooth muscle cell proliferation. IL-8, involved in neutrophil migration and angiogenesis, is produced locally in muscles during exercise with a minimal systemic response observed only after intense exercise. High-exercise loads can also increase circulating anti-inflammatory cytokine IL-10, causing immunosuppression.
Ultimately, professional athletes exhibit an overall pro-inflammatory profile, with different endotypes linked to activity type and intensity. The endurance groups, show a more anti-inflammatory immune profile when compared to the others. In conclusion, advances in omics approaches could offer detailed assessments of athlete health and fitness, enhance our understanding of exercise-immune system interactions, mechanistic processes, functional differences, and pathways associated with various sports. This could also lead to the detection of biomarkers to distinguish between normal recovery and overtraining, ultimately aiming to balance immune health and maximize athletic performance.
Quiz question
After intense exercise which pro- and anti-inflammatory cytokines are expressed and what is their behavior?
IL-8 proinflammatory cytokine is produced with a significant systemic response observed after intense exercise as well as IL-10 which induces immunosuppression.
IL-8 pro-inflammatory cytokine is significantly downregulated after intense exercise while IL-10 is upregulated to induce immunosuppression.
IL-8 pro-inflammatory cytokine is produced with a significant systemic response observed after intense exercise with no significant expression of IL-10.