Introduction
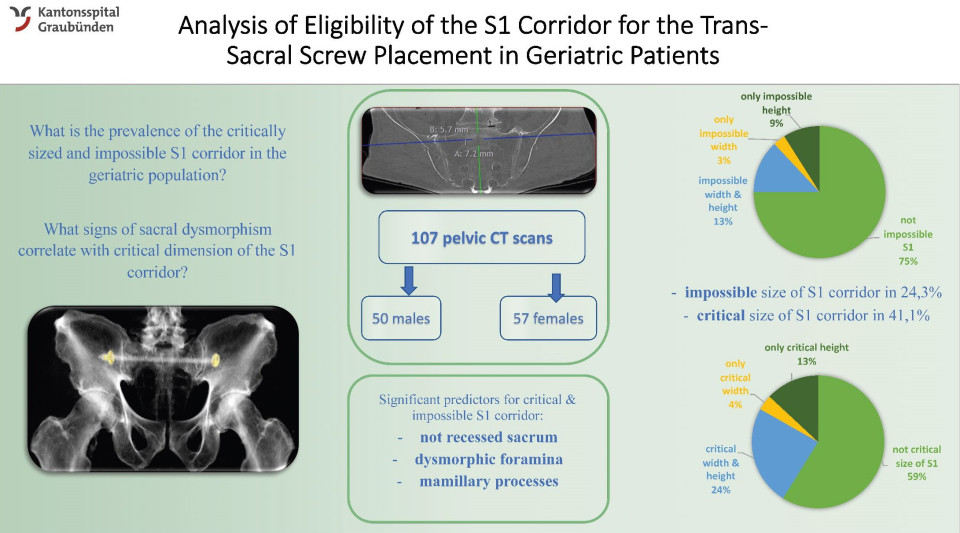
Minimal-invasive placement of a trans-sacral screw represents an increasingly popular method of fixation for Fragility Fractures of the Pelvis (FFP), with variable upper sacral anatomy representing the main challenge. Little is known about the variability of sacral anatomy in the geriatric population and the potential effect of osteoporosis on the upper sacral anatomy and thus S1 corridor morphology. To examine the eligibility (>12 mm) of the S1 corridor for the trans-sacral screw placement in a geriatric population and to analyse what pelvic dysmorphism signs might serve as predictors for an ineligible S1 corridor.
Methods
We analysed S1 corridor in pelvic CT scans of 107 geriatric patients without history of fracture or other pelvic pathology. First, the eligibility for the trans-sacral screw placement was determined by measuring the width and the height of the central portion of the S1 corridor. Then, pelvises were examined for signs of dysmorphism. The correlation of these signs with the ineligible S1 corridor was analysed.
Results
In our geriatric population with average age of 79,55 ± 8.79 years (male:female 0.88) 41% of S1 corridors were not eligible for a trans-sacral screw. In this ineligible group the height was shown to be a more significant limiting dimension (90,9%), compared to the width in 68,2% (p<0.05). Mamillary processes, not recessed sacrum and dysmorphic sacral foramina were present in 38,3%, 34,6%, and 26,2% respectively, with not recessed sacrum demonstrating a significant correlation with a too narrow S1 corridor (p<0.05).
Conclusion
The analysed geriatric population demonstrates a high prevalence of a too narrow S1 corridor, which makes a placement of a trans-sacral screw risky or even impossible. The height of the S1 corridor represents the main limiting factor with a dysmorphism sign of a not recessed sacrum being a significant predictor for the ineligible S1 corridor.
Quiz question
How often is the S1 corridor impossible for the trans-sacral screw fixation in the geriatric population?
It is always possible to perform a trans-sacral screw fixation using the S1 corridor.
In around 25% of the geriatric patients.
In 12% of the geriatric patients the S1 corridor is impossible for the trans-sacral screw fixation.